Joint pathologies are among the most common among all disorders of the musculoskeletal system. Inflammatory and non-inflammatory diseases significantly worsen the quality of human life and in many cases cause disability. One of the most common diseases is osteoarthritis of the knee joint. Symptoms of pathology are more often acute and require specialized help.
Causes of the disease
In medicine, the disease is also called osteoarthritis, gonoarthrosis, deforming osteoarthritis (DOA). Arthrosis is a general name for all degenerative-dystrophic diseases of the articular and intervertebral joints. The violation in the area of the knee joint is called gonoarthrosis.

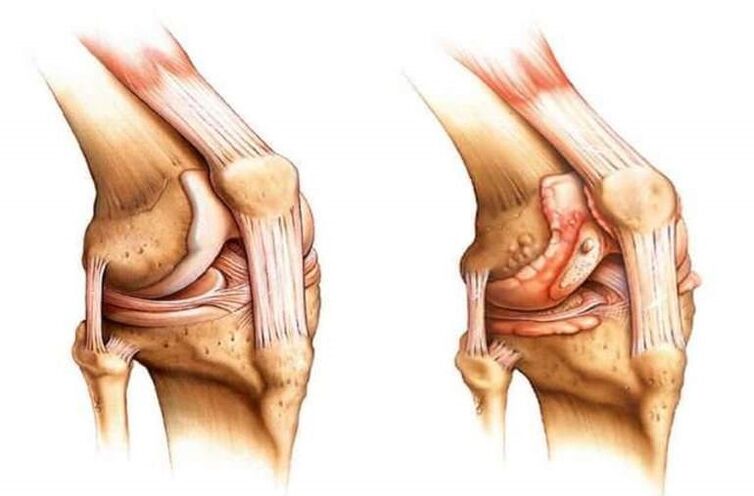
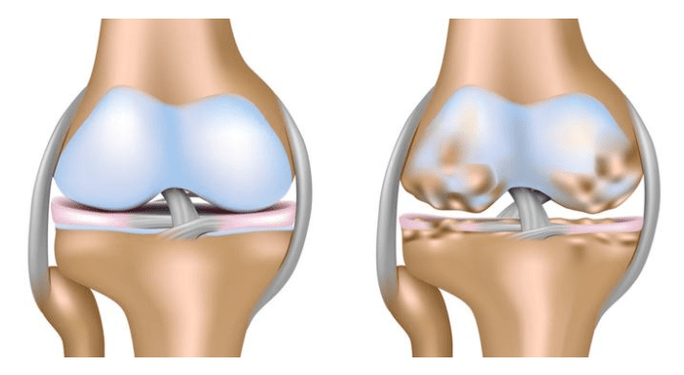
It is characterized by damage to the cartilage in the knee joint.
The pathology consists of degenerative-dystrophic changes in the bone and cartilage tissue, characterized by a gradual thinning of the cartilage in the articular joint and the parallel formation of bony growths.
This becomes the body's reaction to friction and increased pressure. The most likely causes of knee osteoarthritis symptoms are the following:

- Traumatic injuries of mild and severe forms with reduced mobility of the articular joint for a long time. Ligament rupture or severe bruising often causes the development of an inflammatory process, which as a result causes symptoms of gonoarthrosis.
- Surgery on the knee joint to remove any defect or foreign body.
- Prolonged and excessive physical activity on an ongoing basis. This may be due to professional sports or specialty. Constant tension in the joint area leads to a gradual thinning of the cartilage, which negatively affects the entire musculoskeletal system.
- Acute bursitis with development of purulent inflammation in the joint cavity. As a rule, it is difficult to get rid of such a pathology in a conservative way, so doctors resort to minor surgery, which negatively affects the cartilage tissue.
- Arthritis of various forms and severity. In this case, the inflammatory process is intense, proceeds with a sharp increase in temperature and leads to the development of arthropathy after a certain period of time.
- Gout also often leads to cartilage pathology with severe clinical manifestations and joint deformity.
- Weakening of immunity, which causes a gradual resolution of bone and cartilage tissue due to the inability of the body to cope with the pathology.
- Bad habits - alcohol abuse, smoking - quite often become a predisposing factor for the appearance of signs of pathology.
- Serious autoimmune diseases.
- Frequent viral and catarrhal pathologies that cause an inflammatory process and the development of degenerative-dystrophic changes.
- Overweight and severe obesity also cause a violation, since each extra kilogram increases the load on the articular joints by 10 times, which will certainly affect the cartilage tissue.
It is worth noting that all these reasons most often cause a secondary type of violation. There is also a primary one, which differs in that the disease becomes a consequence of the body's natural aging process. Bone and cartilage tissue wears down, which increases friction and stress. The result is gonoarthrosis.
Varieties of pathology
There are several types of pathological conditions, each of which has its own characteristics. Depending on how the joint is affected, the following types of disorders are distinguished:
- The right side is characterized by the appearance of changes in the cartilage tissue on the right side. As a rule, it becomes the initial stage of the disease.
- The signs of the left genoarthrosis of the knee joint by the nature of the clinical picture do not differ from the right side. However, it is noted that this type often develops in overweight patients.
- Bilateral refers to severe forms, affects the entire cartilage and is characterized by severe pain.
It is noted that the latter type is more often observed in elderly patients with primary tissue damage. Depending on the course of the pathological process, acute and chronic types are distinguished. The first is characterized by rapid development and development of complications, the second progresses slowly, may not bother the patient for several years.
Clinical picture
The signs of knee osteoarthritis and its symptoms largely depend on the degree of joint damage. Currently, there are several stages of the pathological process, each of which has its own clinical manifestations:
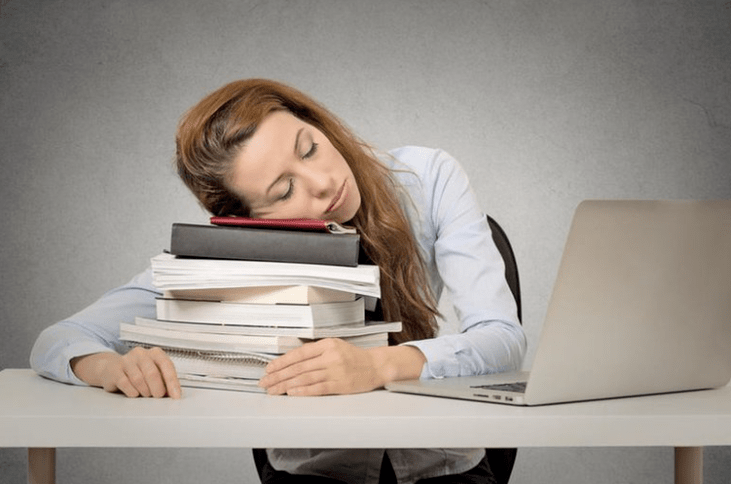

- The initial stage is characterized by the absence of severe symptoms and the inability to visually recognize the pathology. The patient is more tired than usual, but writes it off as overfatigue or increased workload. He becomes lethargic, drowsy and performance drops sharply. Some patients experience mild stiffness in the affected joint when moving, especially in the morning. However, they often do not pay attention to it and do not turn to a specialist. If an X-ray of the joint is taken at this stage, one can observe a narrowing of the joint space, causing a violation.
- In the next stage, discomfort and stiffness do not disappear, but only increase. With a light and short load, the patient develops severe pain in the knee, which disappears only after a long rest. In some cases, the joint swells and this swelling disappears at night, but reappears during the day. Since the pressure on the cartilage tissue increases due to its exhaustion, the patient often hears a characteristic tingling during movements. Flexion function is also impaired, as the patient cannot fully bend the limb. At this stage, patients usually turn to a specialist.
- The third stage is the most serious and is characterized by an intense pain syndrome that accompanies the patient not only during exercise, but also at rest. In severe cases, the pain does not leave a person even at night, which significantly worsens his condition. Swelling at this stage is constantly observed. In the synovial sac, the amount of synovial fluid decreases sharply, which increases the load and increases friction in the joint.
- The initial stage is characterized by the absence of severe symptoms and the inability to visually recognize the pathology. The patient is more tired than usual, but writes it off as overfatigue or increased workload. He becomes lethargic, drowsy and performance drops sharply. Some patients experience mild stiffness in the affected joint when moving, especially in the morning. However, they often do not pay attention to it and do not turn to a specialist. If an X-ray of the joint is taken at this stage, one can observe a narrowing of the joint space, causing a violation.
- In the next stage, discomfort and stiffness do not disappear, but only increase. With a light and short load, the patient develops severe pain in the knee, which disappears only after a long rest. In some cases, the joint swells and this swelling disappears at night, but reappears during the day. Since the pressure on the cartilage tissue increases due to its exhaustion, the patient often hears a characteristic tingling during movements. Flexion function is also impaired, as the patient cannot fully bend the limb. At this stage, patients usually turn to a specialist.
- The third stage is the most serious and is characterized by an intense pain syndrome that accompanies the patient not only during exercise, but also at rest. In severe cases, the pain does not leave a person even at night, which significantly worsens his condition. Swelling at this stage is constantly observed. In the synovial sac, the amount of synovial fluid decreases sharply, which increases the load and increases friction in the joint.

As a rule, the pain disturbs the patient's sleep, he becomes irritable and feels constant fatigue. Appetite weakens or disappears completely, which causes a deterioration in the work of the digestive and cardiovascular systems.
Lack of normal sleep often leads to nervous breakdown, especially in elderly patients or young people engaged in vigorous physical work. Impaired memory and reduced concentration are also a result of insufficient patient rest.
Usually, the pathology progresses without temperature, but in advanced stages, when the cartilage is completely destroyed, the friction of the bones and the pressure between them increases, which causes the inflammatory process.
The body tries to restore balance and reduce the load on the connection. This is why osteophytes or bony growths develop in the joint. They become the cause of deformation in the advanced stages of the pathological process.
The most dangerous complication of such violations will be the complete immobilization of the patient and disability. As a rule, this happens when there is no proper treatment or the symptoms of osteoarthritis of the knee are ignored for a long time.
Diagnostic methods
For an accurate diagnosis, the doctor suggests that the patient undergo a complete examination. This is necessary not only to identify the cause, but also to correctly select the drugs necessary for treatment. The first step will be to interview the patient and identify possible causes. Lifestyle, professional activities and habits play a special role. The next step will be to examine the sick member and determine the degree of damage.

If there are no visible signs of pathology, the disease is at an early stage. The next step will be to collect a history and identify chronic pathologies that could become a predisposing factor. After that, the patient gives blood for laboratory testing. The detection of traces of inflammation in it in the form of an increased level of leukocytes suggests that some process caused the development of the disorder.
An obligatory moment in the diagnosis will be the X-ray examination in order to accurately determine the degree of gonoarthrosis. The image usually shows areas of complete cartilage destruction, as well as the number of osteophytes and their location. This helps to clarify the possible diagnosis and prescribe the appropriate treatment.
Sometimes it is impossible to see the exact picture and degree of joint damage on an X-ray. In this case, it is recommended to undergo an ultrasound examination of the joint.
In extreme cases, the patient is prescribed to undergo a CT scan. This is usually enough to get a complete picture of the disease.
Medical treatment
Conservative treatment of the pathological condition is possible only in the 1st and 2nd stages, when the formation of osteophytes has not yet begun. Treatment is mainly aimed at slowing the destruction of the cartilage and restoring it. The classic scheme includes the use of the following drugs:
- Through the group of pain relievers that help relieve pain. Let the patient feel better, improve night sleep. In a hospital, injections are effective, which are given 1 to 3 times a day under the supervision of a specialist. It is not recommended to use funds for a long time, as they do not affect the course of the pathological process, but only relieve acute pain.
- Non-steroidal anti-inflammatory drugs. Funds are available in tablet and injectable form, they can not only eliminate acute pain, but also slow down the progression of pathology, relieve local fever and swelling, and improve motor function. With regular intake for 7-10 days, a stable concentration of the active components of the drug is observed in the patient's blood, which ensures a prolonged effect. It is not recommended to take drugs for a long time, as they often negatively affect the digestive system. For this reason, they should not be taken by patients with severe peptic ulcers or other disorders.
- Chondroprotectants help restore the cartilage in the affected joint and increase the amount of synovial fluid. As a rule, such drugs contain glucosamine and chondroitin. It is recommended to take them for a long time. Typically, a course of 8-12 weeks is prescribed with regular visits to a specialist to detect improvement. A longer shot with clear indications is possible.
- Glucocorticoids. They are used to treat advanced cases when the pain syndrome is not eliminated by conventional means. It helps relieve swelling and reduce pain. It is allowed to be used only in a hospital in the form of intramuscular or intravenous injections.
- Non-steroidal anti-inflammatory drugs. Funds are available in tablet and injectable form, they can not only eliminate acute pain, but also slow down the progression of pathology, relieve local fever and swelling, and improve motor function. With regular intake for 7-10 days, a stable concentration of the active components of the drug is observed in the patient's blood, which ensures a prolonged effect. It is not recommended to take drugs for a long time, as they often negatively affect the digestive system. For this reason, they should not be taken by patients with severe peptic ulcers or other disorders.
- Chondroprotectants help restore the cartilage in the affected joint and increase the amount of synovial fluid. As a rule, such drugs contain glucosamine and chondroitin. It is recommended to take them for a long time. Typically, a course of 8-12 weeks is prescribed with regular visits to a specialist to detect improvement. A longer shot with clear indications is possible.
- Glucocorticoids. They are used to treat advanced cases when the pain syndrome is not eliminated by conventional means. It helps relieve swelling and reduce pain. It is allowed to be used only in a hospital in the form of intramuscular or intravenous injections.
In addition to such funds, the patient is prescribed a course using an external agent in the form of an ointment, cream or gel. The latter option is more preferable because it quickly penetrates into the joint cavity and has a therapeutic effect. It is allowed to use them within 14 days. It is not recommended to prolong the course yourself, as the risk of complications increases.
In the most severe cases, the patient is injected directly into the joint cavity. You can drive conventional analgesics, but the best therapeutic effect is achieved with the introduction of hyaluronic acid preparations. Injections are given 1 time in 7 days. 3-5 injections are enough to completely eliminate the pain. After such a treatment, the result remains for 6 months. The patient has the ability to move normally and the pain syndrome disappears almost completely.
If none of the methods bring the expected result and the patient's condition worsens, surgery is performed to replace the joint with a prosthesis. Replace the entire link or its individual parts. This is usually indicated for arthropathy, caused by a serious injury to the knee. The operation is performed under general anesthesia, and the recovery period is quite long and difficult.
Gonarthrosis is a serious degenerative-dystrophic pathology, which, if not treated properly, leads to disability of the patient. It is recommended to immediately consult a doctor when the first signs of violation appear.














































